Abstract
Introduction The 2017 European LeukemiaNet (ELN-2017) guidelines for the diagnosis and management of acute myeloid leukemia (AML) have been widely used to assess the risk and prognosis of AML patients. The ELN panels recently updated the latest recommendation in 2022 (ELN-2022). This risk stratification is an expert consensus and lacks real-word validation so far. In this study, we aimed to validate the ELN-2022 risk stratification and proposed possible refinement for a large cohort of de novo AML patients.
Methods and Materials Patients with newly diagnosed non-M3 AML patients, age ranging from 18-65 years, who received standard induction chemotherapy and had adequate bone marrow samples for cytogenetic studies and next-generation sequencing were included. Clinical information, treatment regimen and response, and clinical outcome were collected.
Results A total of 809 de novo non-M3 AML patients were included. Three hundred and twenty-seven (40%), 218 (27%) and 264 (33%) patients were classified to ELN-2022 favorable, intermediate and adverse risk groups, respectively. Adverse-risk patients were older, more often male gender and had lower leukocyte count at diagnosis. Besides those class-defining recurring genetic abnormalities, favorable risk group more frequently had GATA2 and KIT mutations, intermediate risk group had WT1, DNMT3A and TET2 mutations and adverse risk group, PHF6 and IDH2 mutations.
The risk categories of 101 (12.5%) patients were re-distributed from ELN-2017 to ELN-2022, 23 from favorable to intermediate, one from favorable to adverse, 14 from intermediate to favorable, 37 from intermediate to adverse, one from adverse to favorable and 25 from adverse to intermediate-risk.
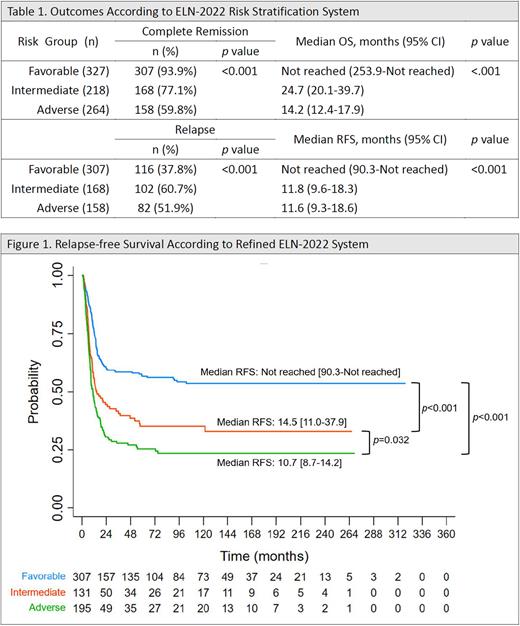
The complete remission (CR) rate was 93.9%, 77.1% and 59.8% and the relapse rate was 37.8%, 60.7% and 51.9% in ELN-2022 favorable, intermediate and adverse risk group, respectively (both p<0.001) (Table 1). With a median follow-up of 112 months, median overall survivals (OS) were significantly different among these three groups: not reached (95% CI 253.9-not reached), 24.7 (20.1-39.7), and 14.2 (12.4-17.9) months, respectively (p<0.001). Median relapse-free survival (RFS) was not reached (95% CI, 90.3-not reached), 11.8 (9.6-18.3) and 11.6 (9.3-18.6) months, respectively (Table 1). Allo-HSCT in first CR was beneficial to intermediate risk patients for both OS (HR with 95% CI; 0.45, 0.27-0.74, p=0.002) and RFS (HR 0.44, 0.27-0.73, p=0.001). In contrast, HSCT showed no survival benefits to favorable and adverse risk patients.
However, ELN-2022 risk stratification seemed unable to well discriminate RFS between intermediate and adverse risk groups. Furthermore, survival analysis of the genetic subsets showed that t(6;9)(p23;q34.1)/ DEK-NUP214, which was categorized as ELN-2022 adverse-risk, was associated with better outcome compared to other patients in the same risk group. On the other hand, t(7;11)(p15;p15)/NUP98-HOXA9, a cytogenetic aberration more common in Asia than in the West, and co-mutated DNMT3A and FLT3-ITD without concurrent adverse-risk genetic abnormalities predicted worse outcome than other patients in the intermediate-risk group. Thus, we proposed a refined ELN-2022 risk stratification, which re-categorized AML with t(7;11)(p15;p15)/ NUP98-HOXA9 and AML with co-mutated DNMT3A and FLT3-ITD without other adverse-risk factors from intermediate to adverse risk group, and AML with t(6;9)(p23;q34.1)/DEK-NUP214 as intermediate risk group. Refined ELN-2022 system worked well not only for OS, but also could better stratify intermediate and adverse groups for RFS [median RFS (95% CI): 14.5 (11.0-37.9) versus 10.7 (8.7-14.2) months, p=0.032] (Figure 1).
Conclusions Our study showed that ELN-2022 could well stratify AML patients into favorable, intermediate and adverse risk groups. These three risk categories had good correlation with CR rate and OS, but relapse rate and RFS were similar between intermediate and adverse risk groups. We proposed a refined ELN-2022 risk stratification, which re-categorized AML with t(7;11)(p15;p15)/NUP98-HOXA9 or co-mutated DNMT3A and FLT3-ITD as adverse risk and AML with t(6;9)(p23;q34.1)/DEK-NUP214 as intermediate risk. Refined ELN-2022 system not only worked well for OS, but also better stratified intermediate and adverse groups in terms of RFS.
Disclosures
Chou:aether AI: Other: The AI product in this abstract... investigators of this study w/commercial profit; National Taiwan University Hospital: Other: The AI product in this abstract... investigators of this study w/commercial profit.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal